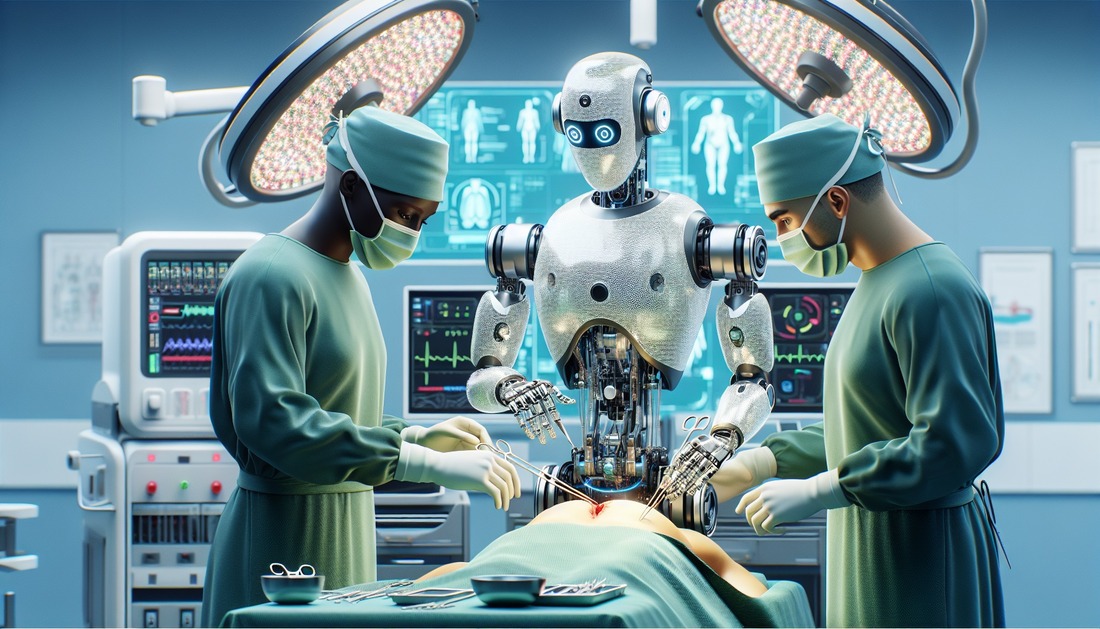
Robotic surgery powered by artificial intelligence (AI) transcends the realm of science fiction; it is revolutionizing the medical field, delivering precise, efficient surgical experiences and improved patient outcomes. With advances in AI algorithms and more intuitive control of robotic equipment, the operating room of the future promises to reduce human error, shorten recovery times, and enable procedures previously thought impossible.
From preoperative planning to real-time intraoperative decision-making, the flexibility of robots combined with the predictive analytics of AI is revolutionizing everything. This article explores the cutting-edge medical technologies, ethical dilemmas, and long-term implications of AI-assisted robotic surgery. Understanding the current state of the art and the direction of innovation can help us navigate the significant changes surgeons and patients will experience in the coming decades.
The Rise of AI in Surgical Robotics:
The application of AI in surgical robotics has advanced significantly since the early days of moving simple robotic arms in predetermined patterns. Today’s AI robots utilize deep neural networks, computer vision, and machine learning to adapt in real time. They can detect problems, assess relevant anatomical data for each patient, and help surgeons perform micro-movements with greater stability than humans. While systems like the da Vinci Surgical System have set the standard, next-generation systems will use predictive models and autonomous navigation to guide surgeries with unprecedented precision. This development results in fewer incisions, less blood loss, and less trauma, significantly improving patient safety and recovery rates.
Using Data for Precision and Customization:
Because AI is data-driven, healthcare must leverage vast databases of genomics, medical imaging, and electronic health records (EHRs). AI-assisted robotic surgery can generate highly personalized surgical plans based on a patient’s specific data. For example, AI can simulate the entire surgical procedure within a virtual 3D model of the patient’s anatomy to identify the safest incisions and instrument paths. Surgeries can be tailored to each patient’s physiology, allowing for more precise interventions and a reduced risk of postoperative complications. This level of personalization is one of AI’s most important contributions to surgical innovation and is unattainable with human intervention alone.
Real-Time Surgical Decision-Making:
Real-time intraoperative guidance is one of the most revolutionary applications of AI in robotic surgery. AI systems continuously monitor live video feeds from the endoscopic camera during surgery, identify abnormalities, and provide the surgeon with corrective measures. This is particularly important in complex surgeries where unexpected problems can arise. For example, AI can instantly identify abnormal tissue morphology, compare it to millions of previous cases, and help determine whether it needs to be removed. This technology is intended to act as a highly intelligent “copilot” that enhances the surgeon’s situational awareness and decision-making, rather than replacing human expertise.
Disadvantages of Autonomous Surgical Systems:
Fully autonomous devices that can perform specific procedures without direct human intervention are one of the long-term goals of AI-assisted surgical robots. Research prototypes have demonstrated the feasibility of tissue dissection, vascular ligation, and autonomous suturing. While these developments are encouraging, the complexity of human anatomy and the diversity of patient conditions limit full autonomy. Shortly, ethical concerns, liability issues, and the need for human supervision will limit the autonomy of robots—robots will only be able to assist surgeons, not replace them. However, there is a clear path toward semi-autonomous and guided autonomous surgery, which could revolutionize surgical efficiency in demanding systems.
The Role of Augmented Reality in AI-Assisted Surgery:
One of the most important aspects of the future of surgery is augmented reality (AR). Combined with AI-driven robotics, AR can project crucial information, such as vessel locations or tumor edges, directly onto the surgeon’s field of view. This enhanced visibility provides unparalleled precision while simultaneously reducing the risk of unintentional damage to healthy tissue. The combination of AR and AI technologies enables dynamic overlays that adapt to the surgical field in real time. For complex procedures such as neurosurgery and cardiovascular interventions, where millimeter errors can make the difference between success and failure, this combination of technologies is likely to become the norm.
Training a New Generation of Physicians:
AI-enabled robotic devices are not only surgical tools but also effective training platforms. Virtual AI simulators can simulate patient-specific surgical environments, enabling risk-free practice. These systems can provide personalized feedback and assess performance criteria such as accuracy, speed, and precision. Data-driven, immersive training environments are therefore replacing the traditional apprenticeship model in medical education. The global adoption of such technologies can help narrow the gap in surgical knowledge between developed and developing countries, and surgeons trained in AI-enabled simulations are better equipped to address real-world challenges.
Regulatory and Ethical Challenges:
While the use of AI in robotic surgery offers many advantages, ethical and legal considerations are also important. We must address concerns about algorithmic bias, data privacy, and liability for surgical errors before implementing AI on a large scale. Regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are actively developing frameworks for evaluating the safety and effectiveness of AI-assisted surgical devices. To ensure informed patient consent, the extent to which AI is used in surgeries must be transparent and adhere to ethical standards. The speed and scope of adoption of new technologies depend on the balance between innovation and safety.
The Way Forward: Outlook for the Next Decade
In the coming decade, assisted precision surgery will give way to collaborative intelligence—a partnership between physicians and AI. Advances in tactile feedback will make operating robotic instruments feel as natural as a surgeon’s hands, while advances in natural language processing will enable surgeons to give voice commands to robots during surgeries. Cloud-based AI systems will enable collective learning, allowing robots worldwide to learn from each other’s experiences. Ultimately, AI-assisted robotic surgery will improve access to advanced medical care worldwide, particularly in resource-poor areas, while simultaneously making complex surgeries safer.
Conclusion:
At the intersection of medical knowledge and computing power, AI-assisted robotic surgery has the potential to provide more precise, personalized, and comfortable surgical care in the future. As the analytical and predictive capabilities of artificial intelligence (AI) continue to improve, robotic systems will become indispensable partners in the operating room. Access to quality medical care will no longer be limited by distance, recovery times will be shorter, and complicated or dangerous surgeries will be less frequent. While many technical, ethical, and legal hurdles remain to be overcome, the benefits are numerous. The precision of robotics, combined with the analytical power of AI, will redefine surgery for the next generation and make healthcare safer, smarter, and more human-centered than ever before.
FAQs:
1. How does AI improve the outcomes of robotic surgery?
AI improves accuracy, reduces human error, and provides real-time support, accelerating recovery and minimizing surgical complications.
2. Is AI-assisted robotic surgery fully autonomous?
Currently, most surgeries are semi-autonomous, with the surgeon maintaining control while AI assists with accuracy and decision-making.
3. Which surgeries benefit most from AI-assisted robotic technology?
Complex procedures such as minimally invasive laparoscopic surgery, cardiac surgery, and neurosurgery offer significant benefits.
4. How does AI-assisted surgery utilize patient data?
Data can be used to predict potential complications, build treatment models, and develop personalized surgical plans.
5. What are the main barriers to widespread adoption?
Regulatory approval, ethical concerns, high costs, and the need for specialized training are among the main obstacles.